Wisdom teeth catch some of our patients by surprise. Many of our young patients in highschool are surprised to learn they have another set of molars about to erupt, remembering that they were in middle school when the last set came in.
They’re called wisdom teeth because they come in quite a bit later than your other adult teeth, usually around the age of adulthood. Understanding how to take care of this set of teeth, whether to extract them and how they might affect the rest of your dental health is paramount—so you or your young adult children aren’t surprised by what x-rays at a dental exam might show.

What Are Wisdom Teeth?
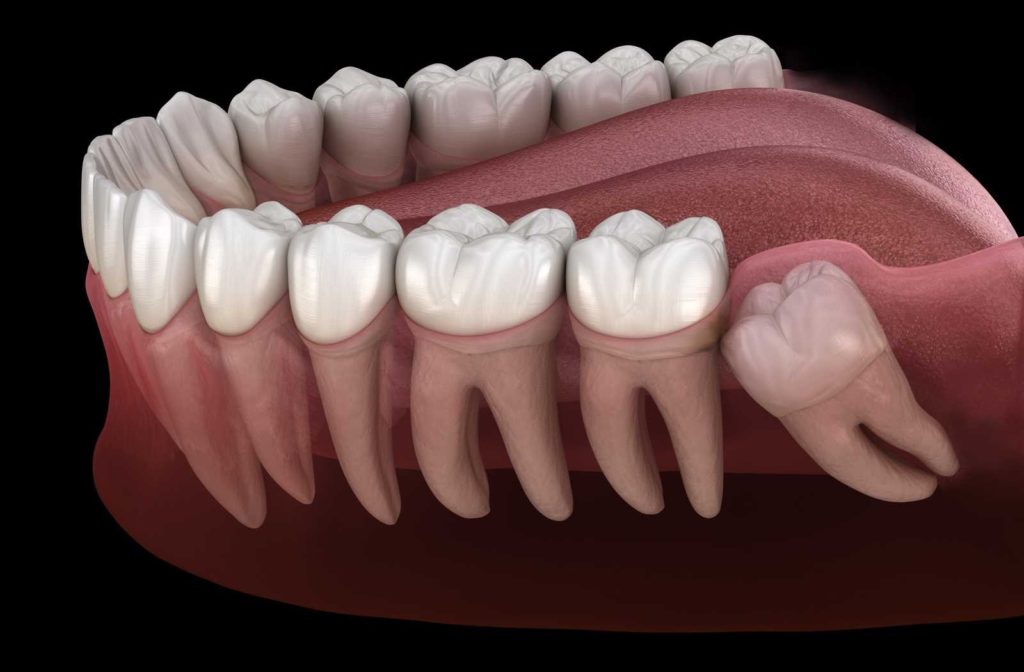
Wisdom teeth are the last teeth you get, usually growing in as you reach adulthood. They’re a set of 4 molars, called 3rd molars, behind 2 other sets or molars, and if they line up well they can be quite useful to you—provided they have space to come in.
Why Wisdom Teeth Need to be Removed
Unfortunately, it’s quite rare that wisdom teeth have enough room to erupt properly. Most of the time, the space they need to come in just isn’t there. In such cases these teeth can cause other problems like cavities, damage to adjacent teeth, gum issues, and more as they are very difficult to keep clean.
Wisdom tooth extractions can also ease up some of the complications of crowding and partial eruption referred to as impacted wisdom teeth.
What if Wisdom Teeth Aren’t Removed?
As mentioned, gum disease can upset your oral health if wisdom teeth are impacted. Crowding can lead to another issue.
Malocclusion
Malocclusion means “bad bite.” A bad bite lacks the alignment needed to bite properly. Some individual teeth can get uneven pressure, as the bite fails to align due to the crowding.
Malocclusion can be expensive and difficult to correct, so wisdom teeth removal is often the simpler option.
Infection
Due to partial wisdom tooth eruption, gum infections are very common. Tooth decay is another common issue as keeping these teeth clean is very difficult.
What to Expect from a Wisdom Teeth Removal Process
It can seem like a daunting prospect, but as long as you work with your dentist and manage your expectations, there’s nothing to fear from a wisdom tooth extraction.
Consultation & X-Rays with Your Dentist
The first step is usually an identification of your wisdom teeth coming in as you reach the ages of 17-25. It’s likely that you won’t have enough room for your wisdom teeth to come in. You might feel a dull pain, but if you don’t yet, it doesn’t mean extraction isn’t necessary. Either way, the x-rays we take can shed light on whether they need removing.
Scheduling an Extraction
Try scheduling an extraction for a week on which you can take a lot of recovery time, and on a day you can get a ride home. We can work with you to manage your expectations of the day the surgery takes place.
On the Day of Your Surgery
Dietary instructions come with anesthesia, so please follow these with care. What you eat can interfere with your body’s reaction to the anesthesia. Nausea and vomiting might threaten your lungs, so it’s imperative you don’t introduce that factor.
Sedation Options
Local anesthesia involves a numbing process with a needle injecting only on the operating site. is an option, but you remain awake for the procedure. Wisdom tooth surgery is invasive, and sometimes the sounds can be unsettling enough to cause the patient significant distress.
Sedation is a sleep-like state where patients are generally unaware of their surroundings but may respond to stimulation. Your dentist may advise on several levels of sedation, usually the amount that carries the least risk:
- Minimal Sedation (anxiolysis)
- Moderate Sedation (analgesia)
- Deep Sedation
The Surgery
How long the surgery takes can vary based on how many wisdom teeth you have and whether they’re impacted. You can ask your surgeon for a time estimate based on your wisdom teeth.
During the surgery, your dentist may have to make cuts into your gums. Then, they’ll proceed with the removal. In many cases, it’s a matter of dividing the tooth into a few pieces and carefully removing the sections.
But sometimes your dentist or oral surgeon might have to drill around the wisdom tooth to remove it fully. Your dentist will then sew stitches over the site after all the teeth have been removed.
Recovery In-Office
Your sedation option and your body’s unique reaction to the anesthesia will impact how much time you need to recover in the office. It could be up to a couple of hours after the surgery if your sedation included general anesthesia. Driving might present a hazard, so you’ll have to wait until we can give you the all-clear.
It might even be hazardous to let you walk downstairs or on sidewalks. We find it’s best to arrange a ride home. Some patients are able to drive themselves home, however. You’ll also get your first set of gauze pads over the wound for recovery at home.
Healing Period
For most, healing is relatively straight-forward, especially if you’re under 25. In cases where you lose some bone material in your jaw, healing can be a process. But in most cases, bleeding subsides within 24 hours.
Pain levels can vary and you may experience some pain for a few days to a few weeks after surgery. Your dentist may prescribe you pain medication to help with the healing process.
Your dentist will have given you a supply of gauze, to help apply pressure to the surgery site. Make sure you put the gauze in wet and behind your last tooth in the back of your mouth.
What to Avoid
Drinking through straws can actually loosen the blood clots at the site of the surgery, so you’ll need to be careful.
Hard food for the first few days after the surgery is not recommended. It can also loosen the blood clots and it could help bacterial infections along if it got lodged in the recovering areas.
Problems to Watch for
You’ll want to keep an eye out for signs of infection. Infections can work their way into the bloodstream if they have the opportunity. If you taste an unusual, tangy flavor, you might need antibiotics. If your dentist prescribed them to mitigate this risk, you should complete taking the full course of oral doses.
Dry socket can be quite common, especially in the lower jaw. It affects patients when a blood clot fails to form, or becomes dislodged. Pain (perhaps severe pain), and a foul odour are signs you’ve got dry socket. Your dentist can treat dry socket by inserting medication into the healing socket.
Paresthesia is a rare complication from the surgery. It refers to nerve damage. Since the wisdom teeth are in the alveolar bone, which houses the nerves and blood vessels running up to each tooth, there’s a risk of nerve damage. Like dry socket, this is more common in the lower jaw.
Nerve damage can be temporary or permanent. But your dentist or oral surgeon will work carefully to avoid the remote chance the extraction could damage these nerves.
Trust Your Dentist
You might be a bit overwhelmed and worried if you’re considering wisdom tooth extraction. The surgery can get quite invasive, and some patients have more difficulty with wisdom tooth extraction than others. But we can guide you every step of the way. If you request a consultation, we can help you manage your expectations.


